Germs may be too small to see, but don't let their size fool you: Certain bacteria and molds are terrifying, causing more than 100,000 American deaths each year. To make matters worse, these microorganisms tend to mutate, becoming impervious to the drugs we've developed to defeat them. How can you spot killer germs before they colonize, invade, and multiply? Read on as we reveal the seven scariest germs,and what you can do to protect yourself.
According to the Infectious Diseases Society, these potentially lethal microbes have exhibited the most harmful drug resistance. Deadly Microbes
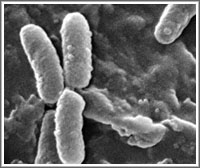 Pseudomonas aeruginosa. Because it rarely causes disease in healthy people, but instead infects those who are already sick or have weakened immune systems, P. aeruginosa is called an opportunistic pathogen.
Pseudomonas aeruginosa. Because it rarely causes disease in healthy people, but instead infects those who are already sick or have weakened immune systems, P. aeruginosa is called an opportunistic pathogen.
These dangerous, antibiotic-resistant bacteria are often spread between medical equipment, sinks, and even food, so hospital patients are a high-risk group. And infection can occur in several sites throughout the body, including the heart and blood, bones and joints, central nervous system, eyes and ears, urinary tract, lungs, and skin.
Fortunately, most hospitals have programs in place for the prevention of nosocomial diseases (infections contracted by patients while under medical care).
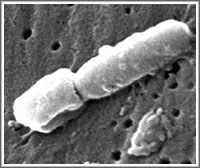 Klebsiella. Regularly found in the human respiratory, intestinal, and urinogenital tracts, Klebsiella are especially important for healthy bowel function. But when they travel outside their normal stomping grounds, serious infection can occur.
Klebsiella. Regularly found in the human respiratory, intestinal, and urinogenital tracts, Klebsiella are especially important for healthy bowel function. But when they travel outside their normal stomping grounds, serious infection can occur.
According to the Centers for Disease Control and Prevention (CDC), Klebsiella infections most commonly occur in people with weakened immune systems and underlying diseases, as well as hospital patients. Some of the most common hospital-acquired infections caused by Klebsiella include surgical wound infections and infections of the blood, and if not treated early enough, both can progress to shock, or even death.
Transmission of Klebsiella infections can be reduced through strict adherence to hospital protocol, including frequent hand-washing.
 E. Coli. Commonly found in the lower intestine of humans and other animals, most E. coli strains are harmless, but certain strains, such as O157:H7, can cause life-threatening conditions such as hemolytic uremic syndrome (often requiring a blood transfusion and kidney dialysis), especially in young children, the elderly, and the immunocompromised.
E. Coli. Commonly found in the lower intestine of humans and other animals, most E. coli strains are harmless, but certain strains, such as O157:H7, can cause life-threatening conditions such as hemolytic uremic syndrome (often requiring a blood transfusion and kidney dialysis), especially in young children, the elderly, and the immunocompromised.
The O157:H7 strain is linked to the 2006 E. coli outbreak of fresh spinach in the United States.
Fortunately, the likelihood of O157:H7 transmission can be reduced by carefully cleaning fruits and vegetables, thoroughly cooking meat, and washing your hands after using the bathroom.
 Vancomycin-resistant Enterococcus faecium (VRE). Enterococci are bacteria normally present in the human intestines and female genital tract.
Vancomycin-resistant Enterococcus faecium (VRE). Enterococci are bacteria normally present in the human intestines and female genital tract.
Typically not dangerous for healthy people with strong immune systems, certain antibiotic-resistant enterococci (like VRE) can cause life-threatening infections in those with compromised immune systems-specifically the very young, very old, and very ill. To date, hospitals are the most documented source of VRE in the United States, according to the CDC.
Careful hygiene is an important part of avoiding transmission of VRE, especially if you're a home caregiver. The CDC recommends washing your hands thoroughly with soap and water after using the bathroom, handling soiled clothing, or preparing food.
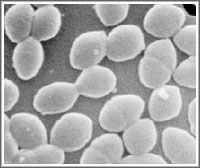
 Drug-resistant Staphylococcus aureus. Resilient spherical microbes that colonize the skin or nostrils of about 20 to 30 percent of the world's population, staph bacteria can also survive for a considerable amount of time on static surfaces, especially in warm and moist areas.
Drug-resistant Staphylococcus aureus. Resilient spherical microbes that colonize the skin or nostrils of about 20 to 30 percent of the world's population, staph bacteria can also survive for a considerable amount of time on static surfaces, especially in warm and moist areas.
The bacteria are often spread through skin contact and are harmless until they enter the bloodstream. Then they can cause infections as deadly as pneumonia, meningitis, or septicemia.
Overuse of antibiotics has led to the emergence of drug-resistant forms, such as methicillin-resistant Staphlyococcous aureus (MRSA), which can be treated with vancomycin, though recent strains that are less responsive to that antibiotic have surfaced.
To protect yourself against MRSA, which causes 19,000 deaths annually according to the Centers for Disease Control and Prevention, wash your hands frequently, use antibiotics properly, avoid sharing items that come in contact with the skin, and keep wounds clean and covered.
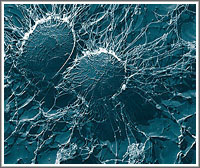
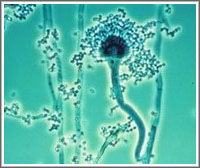 Aspergillus. This mold, which plays a crucial role in the breakdown of organic matter, is almost everywhere, and therefore, unavoidable.
Aspergillus. This mold, which plays a crucial role in the breakdown of organic matter, is almost everywhere, and therefore, unavoidable.
Most types are harmless, but for people with weakened immune systems or lung diseases, certain specimens of Aspergillus can cause aspergillosis, a group of infections that can be deadly. In 50 to 90 percent of cases involving invasive aspergillosis (the most severe form), the outcome is death, especially if the illness develops drug resistance and the patient suffers from another disease such as AIDS or cancer.
Fortunately, a medical breakthrough came in 2005 when British researchers were able to decipher Aspergillus's genetic code, which will potentially lead to more effective treatments.
Acinetobacter baumannii. Because it's extremely drug-resistant and able to exist at numerous temperatures and pH levels, this bacterium poses a palpable threat in hospitals, where a majority of the people affected contract the bug.
As with Aspergillus and MRSA, A. baumanni is especially dangerous to people who are already ill. Causing pneumonia, meningitis, and blood and wound infections, it has a mortality rate as high as 75 percent.
A. baumannii infections are often treated with polymyxins or imipenem, an antibiotic that carries a risk of seizures.
7 Germs That Kill
By Danielle Dowling
Reviewed by QualityHealth's Medical Advisory Board
Updated: November 20, 2008
RELATED HEALTH CENTERS
Explore Original Articles About...
Quick Links:
Health Centers:
ADD/ADHD
Allergies
Alzheimer's Disease
Anxiety
Arthritis
Asthma
Autism
Bipolar Disorder
Breast Cancer
Cancer
Caregiving
Children's
Cholesterol
Colds & Infections
COPD
Crohn's Disease
Dental & Vision
Depression
Diabetes
Diet & Weight Loss
Eating & Nutrition
Epilepsy
Erectile Dysfunction
Fitness & Exercise
Flu Treatment
Healthy Aging & Retirement
Heart Health
Heartburn & GERD
IBS
Incontinence
Men's Health
Meningitis
Menopause
Mental Health & Addiction
Migraines & Headaches
Multiple Sclerosis
Osteoporosis
Pain Management
Parkinson's Disease
Pregnancy
Relationships & Emotional Health
Sexual Health
Skin Care & Beauty
Sleep Management
Smoking Cessation
Stomach & Digestive
Women's Health
|
|  |
|




